Everyone is aware that the rates of Cesarean deliveries all over the worldwide are alarmingly high, particularly in middle- and high-income countries without evidence indicating substantial maternal and perinatal benefits from the increase and some studies showing negative consequences for maternal and neonatal health. The lack of a standardized internationally-accepted classification system to monitor and compare CS rates in a consistent and action oriented manner is one of the factors that has hindered a better understanding of this trend.
Why classify Cesarean deliveries?
A common acceptable classification of Caesarean delivery rates and indications allows evaluation and comparison of the contributors to the Caesarean section rate and their impact. It also allows comparison between institutions, regions, and countries that adopt this classification.
Any such classification should be
- Simple
- Relevant clinically
- Accountable
- Reproducible
- Verifiable
- Mutually exclusive
CS classifications are of three types
- Indication based (traditional): it is very cumbersome and has limitations
- Degree of urgency: also has several drawbacks
- Woman-based: Robson classification. Systematic reviews have conclude that this is best classification to meet the current need and is recommended the most
- Others
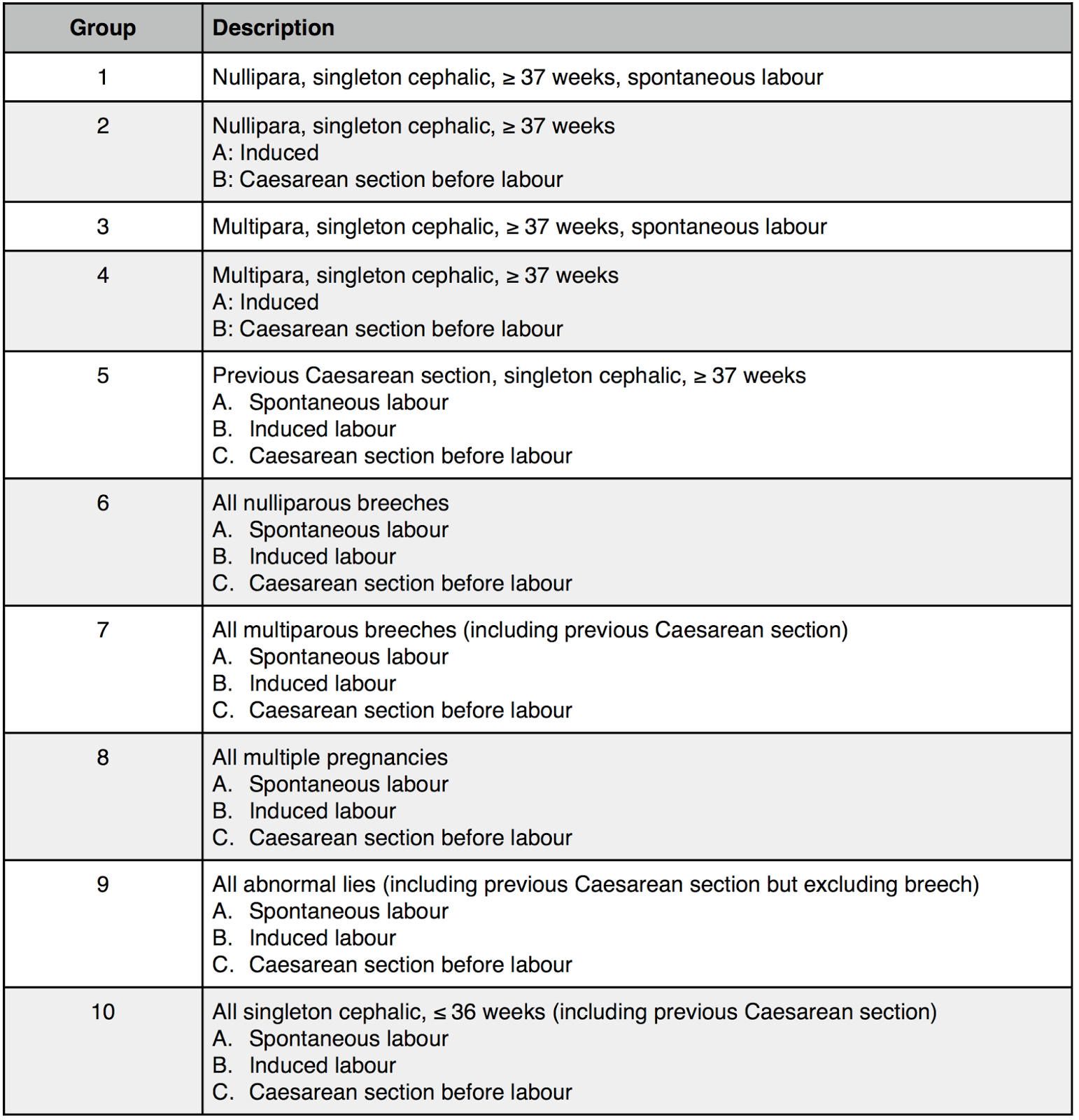
In 2001, Robson proposed a classification (which is also called the the 10-group classification).
It is a system that classifies women into 10 groups based on their obstetric characteristics
- Parity,
- Previous CS,
- Gestational age,
- Onset of labour,
- Fetal presentation and the
- Number of fetuses
Since the system can be applied prospectively and its categories are totally inclusive and mutually exclusive, every woman that is admitted for delivery can be immediately classified based on these few basic characteristics which are usually routinely collected worldwide in obstetric wards.
One noticeable feature of this classification is that it does not use indication for the CS. This allows for the creation of subdivisions in each group and can improve analysis of local practices.
Subdivisions have been proposed for each of the 10 groups but group 5 (women with previous CS) is the group receiving the largest number of suggestions.
Another noteworthy suggestion is the creation of group “99” to include women with missing data and thus unable to be classified in any of the 10 groups.
Instead of mentioning the original classification, I will reproduce the modification of Robson classification by SOGC which I find more useful.
Drawback
A problem with the women-based classifications is that they do not present why (indications) or when (degree of urgency) the CS was performed, which are also important aspects.
Acceptability
Despite the lack of any official endorsement or formal guidelines, the international use of this classification is increasing rapidly and spontaneously.
Conclusion
The use of a single CS classification, such Robson classification in its original form or modified form (SOGC modification) will facilitate auditing, analyzing and comparing CS rates across different settings and help to create and implement effective strategies specifically targeted to optimize CS rates where necessary.
Citations:
- Robson MS (2001) Classification of caesarean sections. Fetal and Maternal Medicine Review 12: 23–39.
- Torloni MR, Betran AP, Souza JP, Widmer M, Allen T, et al. (2011) Classifications for Cesarean Section: A Systematic Review. PLoS ONE 6(1): e14566. doi:10.1371/journal.pone.0014566
- Classification of Caesarean Sections in Canada: The Modified Robson Criteria. http://sogc.org/wp-content/uploads/2013/02/gui281CO1210E.pdf